Good Pharmacy Practice
The health of the public is fundamental to the happiness and welfare of all people & Medicines are an essential and critical part of healthcare services.
There is a gap between the proven efficacy of medicines demonstrated in clinical trials and their actual effectiveness in practice. The reasons for this gap include problems with:
- Medicine selection and dosages,
- Improper administration of medicines and lack of adherence by patients to prescribed treatment,
- Medicine–medicine and medicine–food interactions, adverse medicine events.
- Besides clinical problems associated with medicine-related problems, there are; cost implications.
As health-care professionals, pharmacists play an important role in closing the gap between the potential benefit of medicines and the actual value realized. To reduce such types gaps, International Pharmaceutical Federation (FIP) has been developing guidelines time to time.
In 1992 the International Pharmaceutical Federation (FIP) developed standards for pharmacy services under the heading “Good pharmacy practice in community and hospital pharmacy settings”.
Mission of good pharmacy practice
- is to contribute to health improvement
- is to help patients with health problems to make the best use of their medicines.
- There are six components to this mission:
- being readily available to patients with or without an appointment;
- identifying and managing or triaging health-related problems;
- health promotion;
- assuring effectiveness of medicines;
- preventing harm from medicines; and
- making responsible use of limited health-care resources.
Definition of Good Pharmacy Practice/GPP
Good Pharmacy Practice (GPP) defines- pharmacists provide quality pharmacy service to every patient. It is the practice of pharmacy that responds to the needs of the people, who use the pharmacists services to provide optimal, evidence based care.
GPP is the practice of pharmacy that responds to the needs of the people who use the pharmacists’ services to provide optimal, evidence-based care.
Aim of the Good Pharmacy Practice Guidelines is to set standards for practice of pharmacy as a profession in community pharmacies. GPP is a dynamic concepts.
Good Pharmacy Practice (GPP) organizes following major roles for pharmacists:
- Prepare, obtain, store, secure, distribute, administer, dispense and dispose of medical products.
- Provide effective medication therapy management.
- Maintain and improve professional performance.
- Contribute to improve effectiveness of health care system and public health.
Requirements of good pharmacy practice
- GPP requires that a pharmacist’s first concern in all settings is the welfare of patients.
- GPP requires that the core of the pharmacy activity is to help patients make the best use of medicines. Fundamental functions include the supply of medication and other health-care products of assured quality, the provision of appropriate information and advice to the patient, administration of medication, when required, and the monitoring of the effects of medication use.
- GPP requires that an integral part of the pharmacist’s contribution is the promotion of rational and economic prescribing, as well as dispensing.
- GPP requires that the objective of each element of pharmacy service is relevant to the patient, is clearly defined and is effectively communicated to all those involved. Multidisciplinary collaboration among health-care professionals is the key factor for successfully improving patient safety. In satisfying these requirements, the following conditions are necessary:
- the well-being of patients should be the main philosophy underlying practice, even though it is accepted that ethical and economic factors are also important;
- pharmacists should have input into decisions about the use of medicines. A system should exist that enables pharmacists to report and to obtain feedback about adverse events, medicine-related problems, medication errors, misuse or medicine abuse, defects in product quality or detection of counterfeit products. This reporting may include information about medicine use supplied by patients or health professionals, either directly or through pharmacists;
- the relationship with other health professionals, particularly physicians, should be established as a therapeutic collaborative partnership that involves mutual trust and confi dence in all matters relating to pharmacotherapy;
- the relationship between pharmacists should be one of colleagues seeking to improve pharmacy service, rather than acting as competitors;
- in reality, organizations, group practices and pharmacy managers should accept a share of responsibility for the defi nition, evaluation and improvement of quality;
- the pharmacist should be aware of essential medical and pharmaceutical information (i.e. diagnosis, laboratory test results and medical history) about each patient. Obtaining such information is made easier if the patient chooses to use only one pharmacy or if the patient’s medication profi le is available;
- the pharmacist needs evidence-based, unbiased, comprehensive, objective and current information about therapeutics, medicines and other healthcare products in use, including potential environmental hazard caused by disposal of medicines’ waste;
- pharmacists in each practice setting should accept personal responsibility for maintaining and assessing their own competence throughout their professional working lives. While self-monitoring is important, an element of assessment and monitoring by the national pharmacy professional organizations would also be relevant in ensuring that pharmacists maintain standards and comply with requirements for continuous professional development;
- educational programmes for entry into the profession should appropriately address both current and foreseeable changes in pharmacy practice; and
- national standards of GPP should be specifi ed and should be adhered to by practitioners.
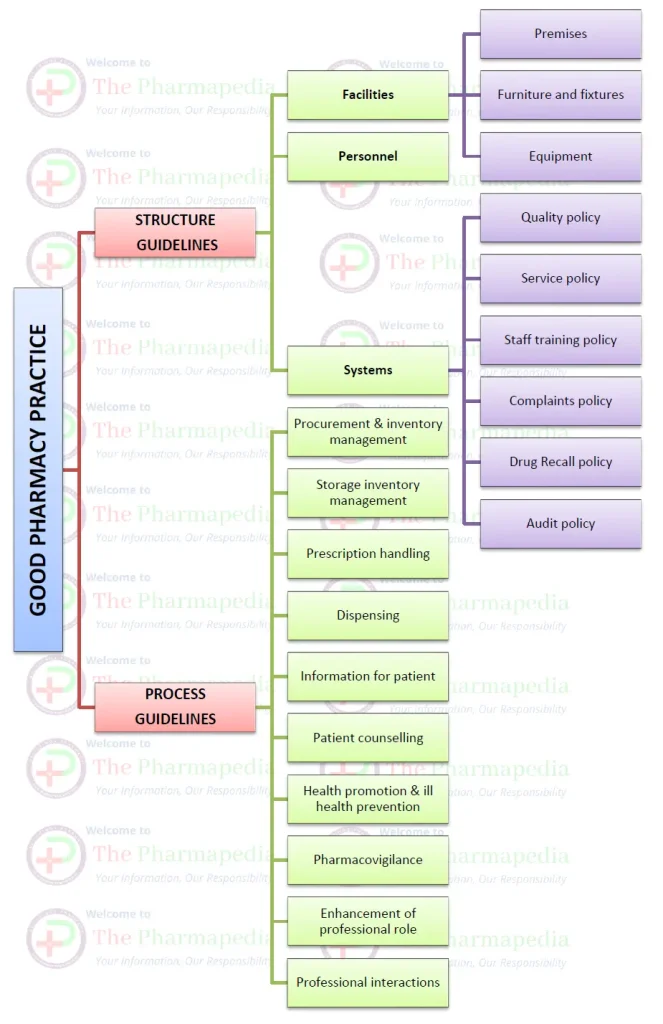
Good Pharmacy Practice (GPP) Guidelines
- Premises/layout
- Furniture
- Equipment
- Manpower
- Material
- Documentation
- Inventory control
- Storage
- Services
1. REQUIREMENTS OF PREMISES/LAYOUT
- The location of pharmacy should be such that it is easily identified by the public.
- The environment in the pharmacy should be neat and clean.
- It should have clearly marked word “PHARMACY” written in English as well as local language.
- The pharmacy should also be accessible to disabled people or people using wheel chairs.
- It should have display counter, shelves for medicine storage, counselling area, waiting area, billing area, adequate space for movement and waste collection boxes
- Counselling area should have furnitures (table and chairs) for comfortable conversation or communication and cabinets for keeping Patient Medication Records (PMR).
- It should have telephone service, electronic supply, refrigerator, drinking water, etc.A compounding pharmacy for extemporaneous preparations should have additional space and necessary equipment.
- An extemporaneous preparation (compound) is a drug or mixture of drugs prepared or compounded in a pharmacy according to the order of a prescriber. Extemporaneous compounding is necessary to treat patients whose needs can’t be fulfilled by commercially produced medications
2. REQUIREMENTS OF EQUIPMENTS
- The pharmacy should be equipped with refrigerator for storage of medicines in cold temperature and validated from time to time.
- Counselling area should be equipped with demonstration charts, patient information leaflets (PILs), reference materials and other required materials.
- It should contain basic instruments like sphygmomanometer, glucometer, thermometer, stethoscope, weight and height scale
- The pharmacy should be preferably equipped with computer and appropriate softwares that can manage inventory, manage invoicing, generate timely warnings for expiring medicines and archive patient medication records.
- Compounding pharmacy should be equipped with appropriate apparatus required for the preparation.
3. REQUIREMENTS OF MANPOWER
- The pharmacy should be managed under the supervision of pharmacist and other personnel working in the pharmacy should be well trained.
- The pharmacy should have well documented guidelines and procedures for personnel set by management with pharmacist consultation.
- The personnel in the pharmacy should wear neat apron/coat and wear a badge displaying name and designation.
- All pharmacy personnel should be medically examined and adequately immunized periodically and their health data should be archived.
- Pharmacist working in the pharmacy should hold at least a bachelor degree in pharmacy and registered as Pharmacist in Pharmacy Council.
- Pharmacist should also have done adequate practical training in community pharmacy and have adequate communication skills for patient counselling.
- Pharmacy Assistant working in the pharmacy should hold at least a diploma in pharmacy and registered as Pharmacy Assistant in Pharmacy Council. Pharmacy Assistant should also have done adequate practical training in community pharmacy and have adequate communication skills.
- Professionalist working in the pharmacy should hold the qualification specified by Drug Advisory Committee and recognized by that committee.
4. REQUIREMENTS FOR STORAGE
- • All medicines coming into the pharmacy should initially be quarantined and then checked for quantity, batch number, expiry, integrity, etc. After checking they should be transferred to their respective storage location.
- • All medicines should be stored at appropriate temperature protecting from excessive light, dust and humidity. Record of daily temperature should be kept in record sheet and preserved for future record.
- • The medicines and shelves should be clean and dust free following Standard Operating Procedures (SOPs).
- • All medicines that are to be stored in cold temperature should be kept in the refrigerator.
- • Narcotics and Psychotropic drugs that fall into Group “X” should be kept in a separate safe with lock andhandled only by the Pharmacist. Records of such drugs should be maintained as per legal requirements.
- • Shelves should be checked periodically for expiry of medicines and expired medicines should be keptseparately labelling “Expired Goods-Not For Sale”.
- • Near expiry medicines which can expire during the prescribed time should not be sold. Expired medicines, unused or unopened medicines are either returned to the supplier or destroyed as per in house protocol.
5. REQUIREMENTS OF INVENTORY CONTROL
- The pharmacy should develop and maintain safe, effective, operational and socioeconomically acceptable procurement and inventory management. Pharmacist should ensure medicines and health care products are readily available in the pharmacy in sufficient quantities.
- Suppliers and Purchasing The pharmacist should ensure quality supply of medicine by purchasing from supplier that meets the standard laid down by the law. Details of suppliers (name, address, contact number, licenses, etc.) should be kept. A list of trusted suppliers should be maintained and visited from time to time for audit of premises and system. Any errors made by the supplier should be reported and rectified in timely manner.
- The pharmacist should inform regulatory authorities if any deliberate dubious activity by the supplier is found.
- The pharmacy should have written procedure for the selection of medicines and maintain product list with retail price including essential and life saving medicines. The product list should be reviewed from time to time and updated by the pharmacist.
- All the medicines received from the supplier should be checked for quantity, price, batch number and expiry date
- Cost effective purchasing method should be followed and the purchase records/invoice should be maintained
6. REQUIREMENTS OF SERVICE
- The pharmacy should have well documented service strategy based on its goals.
- Service strategies includes home delivery of medicine, special care and attention to patients like elderly patients, regular patients, etc.
- Service manual should state in detail service offered, service time and pharmacy operation schedule.
- Service manual should enlist details of activities, routines, delegations, work procedures and instructions for day to day activities in pharmacy.
7. REQUIREMENTS OF DOCUMENTATION
- Documentation is one of the core activities for maintaining and achieving quality.
- Pharmacist should maintain all necessary statutory documents like regulatory licenses, registrations, permissions, etc. for operating a pharmacy and displayed if required under the law.
- All operational documents like purchase invoices, sales invoices and other statutory documents should be maintained and archived as prescribed by law.
- Some of the necessary documents includes:
- Quality manual and policy documents
- Protocols
- Standard Operating Procedures
- Cleaning and maintenance processes and records
- Training manual and training records
- Complaint records
- Audit records
- Personnel details and job descriptions
- Record of narcotics and psychotropics
- Additionally, documents for pharmaceutical care should be adequately maintained and stored. These documents includes:
- Patient’s health profile
- Patient’s medication record
- Record of counselling, follow-ups, etc
Good Pharmacy Practice (GPP) Guidelines (summery)
You may also like…
Bibliography

Comments are closed